December 2022
The INTERREG VA Acute Hospital project closure celebration event took place at South West Acute Hospital in Fermanagh in October. The hybrid session, entitled ‘Resetting Cross Border Delivery of Transformative Acute Services in a Post-Pandemic Healthcare Environment’, enabled delegates to learn more about the project outcomes from key stakeholders and included strong endorsement messages from Minister Robin Swann, Department of Health, Northern Ireland; Stephen Donnelly, Minister for Health, Republic of Ireland; and Dr Margaret Whoriskey, Digital Health & Care Directorate, Scottish Government. SEUPB’s Chief Executive Officer, Gina McIntyre also attended the event and commended the project for achievements and challenges overcome and making a difference to many people’s health and well-being in the border region.

From left: Seán Murphy, General Manager, Letterkenny University Hospital; Neil Guckian, Director General, CAWT and Chief Executive, WHSCT; Mary McMenamin, Acute Services Project Manager; and Ray Nethercott, Consultant Paediatrician, Women and Children’s Services, WHSCT
A facilitated discussion – led by Seán Murphy, Letterkenny University Hospital General Manager – also enabled the sharing of perspectives from those most closely associated with the project, including clinicians and a service user.
Delegates learned that more than 17,000 people from Northern Ireland, the Republic of Ireland and Scotland benefited from the cross border acute services project and its range of transformational initiatives over a wide range of treatment areas including cardiology, respiratory, dermatology, urology and vascular services.
Through the Community Paramedic project – delivered across all three jurisdictions – community paramedics undertook specialised training to enable them to see and treat patients in their communities and their own homes, rather than having to transport them by ambulance to await treatment in busy hospital Emergency Departments. During COVID-19, the service proved invaluable in reducing attendance and admissions to hospital, particularly among the frail elderly.
The project also made a positive, practical impact on internal A & E processes throughout the project. This included the establishment of discharge lounges in Sligo University Hospital, Letterkenny University Hospital and South West Acute Hospital in Enniskillen. These lounges enabled patients to prepare for discharge from hospital in a safe environment, whilst simultaneously supporting staff to create more efficient patient flows, allowing an increased number of patients awaiting bed allocation to be transferred to a ward.
A Clinical Decision Unit (CDU)/Direct Access Unit was established at Daisy Hill Hospital in the Southern Trust area, enabling fast and efficient cross border access to assessment and diagnostics via direct referrals from GPs and other health care professionals. This enabled greater efficiency for emergency admissions for those patients with high acuity conditions.
An important achievement for the project has been the provision of training to 875 staff in a broad range of areas including paramedicine, mentoring development, patient flow, dermatology specialist practice, leadership etc. This enhancement to staff skills will benefit the health services beyond EU funding.
The project is still delivering services in a small number of surgical specialties and will be drawing to a close in the coming weeks.
July 2022
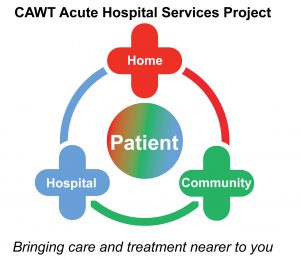
The Acute Hospitals project, aimed at assessing and treating more patients more effectively through improved or reformed service delivery models, is enabled by the establishment of cross border frameworks for scheduled and unscheduled care across Northern Ireland, the border counties of the Republic of Ireland and the West Coast of Scotland. The project has continually evolved, informed by good practice and lessons learned. Since its inception, 17,000 plus patients have benefited from innovative acute services in a range of clinical fields such as cardiology, dermatology, urology, vascular and respiratory care.
In recent months, urology services have benefited significantly from the procurement of a number of outstanding capital items to enable clinicians to deliver high quality interventions to patients.
The project’s urology services in the WHSCT are delivered in four outpatient clinics – Altnagelvin Hospital, Omagh Hospital and Primary Care Complex, South West Acute Hospital (SWAH) and Roe Valley Hospital – and the services work closely with Causeway Hospital, extending the catchment population right up to Ballycastle. In the HSE EU funded urology services had been delivered in Letterkenny University Hospital.
The Urology team tests for and treats a range of kidney, bladder and urine conditions as well as men’s health problems, providing patients with an initial diagnosis and treatment plan.
Mary McMenamin, Acute Services project manager, explained: “Through the Acute Hospital project urology strand, we have been able to offer a range of therapies to support patients with both uncomplicated or very complex needs. Alongside specialist clinics in continence or catheterisation, we now have the technology to offer a new therapy, known as sacral neuromodulation, that may be able to help certain people who experience bladder and bowel problems and who have not improved with traditional remedies such as lifestyle and dietary changes or medication. Where successful, the treatment can be life changing.”
Another significant and recent milestone is the installation of a specialist operation table in SWAH. The height adjustable Merivaara Grand Promerix Operation Table – manufactured in Finland – has been designed to improve ergonomics in surgical procedures.
For patients requiring complex urology surgery it offers comfort and safety, works with smart controls and meets the specific requirements of the hospital environment, allowing staff to focus on the procedure itself.
In addition, the new state-of-the art camera stacks have been purchased to support vital keyhole surgery carried out at the SWAH . The cameras provide clearer images, have much larger screens than previous cameras and also enable staff to record operations so they can be reviewed later and used for training.
May 2021
With over 14,000 patients assessed and treated to date in services such as Dermatology, Vascular, Community Paramedic Services, Cardiac Investigations, Clinical Decision Unit etc., the Acute project is edging its way towards it overall target of 15,000 patients. This has been achieved through the commitment of the CAWT partner organisations throughout the eligible area during the most challenging global health care crisis the world has faced in over 100 years. The health service has learned new ways of working to deliver high quality safe services to patients.
The various strands established within the Acute Project are progressing well. Following the autumn/winter Covid surge all but one service area has fully resumed in providing health care services. Work continues on the completed strands to mainstream or continue such services using the lessons learned during the pilot project phase. This has resulted in many more patients continuing to benefit from of new innovative acute services in their own areas.
Currently, the Project staff team is focusing on supporting the cross-border Urology Services in the Western Health and Social Care Trust and Letterkenny University Hospital, which will see Consultants employed in both partner areas providing services in both jurisdictions.
December 2020
All Strands of the INTERREG VA Acute Project are now established and the project has assessed and treated over 12,000 unique beneficiaries.
The EU funding for a number of services has now been expended, for example, the Community Paramedic work stream. Mainstreaming plans to support these projects are well developed.
The acute hosptial response to Covid-19 requires health professionals to ‘learn to live’ with Covid alongside their clinical practice. The introduction of new cleaning regimes, using additional PPE, and virtual reviews allow services to continue even though the threat of Covid 19 remains. Continuity of these new ways of working in the acute healthcare environment will ensure the delivery of as many services as possible, to as many patients as possible, throughout the eligible area.
For further information on CAWT’s Acute Hospital Services Project contact Louise Potts, Project Manager, email: louise.potts@hse.ie.
August 2020
The INTERREG VA Acute Project has now assessed and treated 9,028 unique patients (well over half of the overall 14,500 target) across a number of different strands throughout the eligible area. Over 640 staff have been trained in the delivery of high quality services in innovative ways. Development of staff is a key objective of the Acute Hospital Services Project; the target set for this objective has now been exceeded.
 The National Ambulance Service Community Paramedic Project made the shortlist for the prestigious 2020 HSE Health Services Excellence Awards. Designed to showcase and celebrate the excellent work delivered by HSE staff, the focus of the Awards this year was sharing good practice and promoting shared learning. Having made the shortlist from over 600 submissions project staff were delighted to be recognised for their innovative and sustainable approach to health care in the community.
The National Ambulance Service Community Paramedic Project made the shortlist for the prestigious 2020 HSE Health Services Excellence Awards. Designed to showcase and celebrate the excellent work delivered by HSE staff, the focus of the Awards this year was sharing good practice and promoting shared learning. Having made the shortlist from over 600 submissions project staff were delighted to be recognised for their innovative and sustainable approach to health care in the community.
The Community Paramedics Project has successfully assessed and treated over 3,000 patients in their own homes and communities. Feedback from a recent patient experience survey indicates that all patients (100%) were extremely satisfied with the quality of care they received by these health professionals. The NI Ambulance Service and the National Ambulance Service have plans in place to continue these unique roles within their Ambulance services following the completion of funding for this successful project. Both organisations are starting recruitment campaigns for additional Community Paramedics. With plans for these additional practitioners to be in post by autumn 2020, other areas on the Island of Ireland will avail of the same service afforded to patients in the project pilot locations.
Service developments within the Pre-hospital Care strand of the Acute Project are well established. These include the Community Cardiac Investigations Service (Sligo/South Fermanagh), the Direct Access Unit (in Daisy Hill Hospital in the Southern Health and Social Care Trust) and the introduction of the Community Respiratory Consultant Service (Sligo) in April 2020. All the Pre-Hospital Care Strands of the Acute Project are providing much needed services on the ground to patients in all three jurisdictions. The evaluation of Patients’ Experiences of the Community Cardiac Investigations Service is complete and the analysis of the surveys is underway.
The Acute Dermatology, Vascular and Urology Strands are now established in at least one, if not two jurisdictions, and contribute to achieving the overall patient beneficiary target required in the Acute Project. Discussions have commenced with our Scottish partners to continue with the National Improvement Nurses Dermatology Education programmes following the conclusion of the funding of this strand of the project.